Valley Health is a not-for-profit organization serving the healthcare needs of Virginia, West Virginia, and Maryland residents. Valley Health provides outstanding care to its patients through a system of six hospitals and related facilities, offering patients convenient care close to home. One of the Valley Health locations is Winchester Medical Center, in Winchester, Virginia. Winchester Medical Center is a 495-bed Level II Trauma Center, Level III Neonatal Intensive Care Unit (NICU), Level 4 Epilepsy Center, Chest Pain Center, Advanced Primary Stroke Center, and a Magnet Designated Hospital. Winchester Medical Center is a resource for more than 500,000 residents, offering diagnostic, medical, surgical, and rehabilitative care and advanced critical care services in heart, neurosurgery, oncology, trauma, and neonatal care.
A Unique Approach to Managing Patient Pain Integrates Amtelco’s On-Call Scheduling Software and the GetWellNetwork System
Helping patients manage their pain is important to every healthcare facility. Being able to monitor and record each patient’s pain level on an ongoing basis can be challenging, as it takes a large amount of a nurse’s time.
Lorraine Leake, Former Corporate Director of Communications at Valley Health, Winchester Medical Center commented, “The ongoing charting takes away time from the patient. Our goal is to do anything we can to help our nurses stay bedside.”
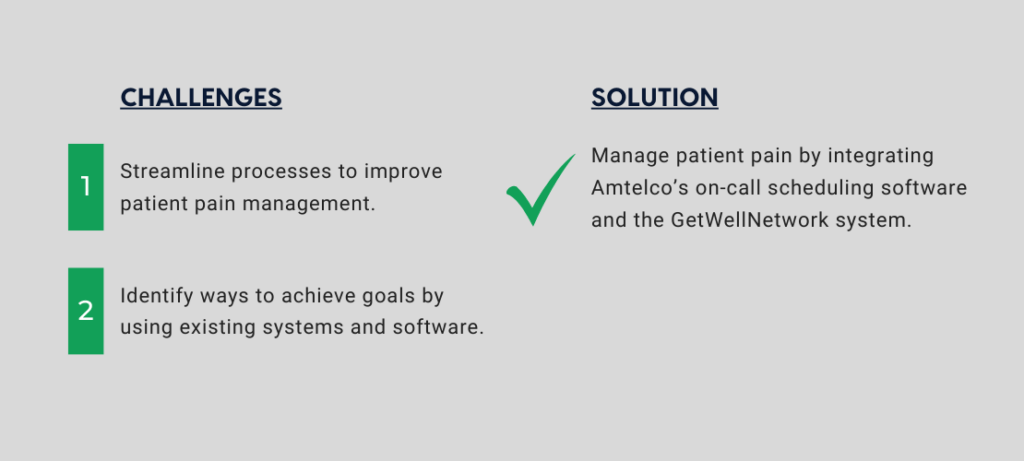
Lorraine looked at the various systems available in their facility to find an easier way for nurses to monitor pain levels. The organization already used Amtelco’s highly interoperable contact center software to streamline enterprise-wide communications, and Amtelco’s system contained real-time patient room and on-call scheduling information. They also used the GetWellNetwork which enables patients to enter their pain level with a remote control. Lorraine presented her ideas about integrating and merging the data within these systems to both Amtelco and GetWellNetwork. The two companies then worked together to integrate the two systems.
How the Pain Pathway Process Works
To start the pain pathway process, a nurse scans a medication given to a patient. Fifty minutes later, the patient is asked to rate their current pain level on a scale of 0 (low) to 10 (high) using the GetWellNetwork on their television. The result is sent through the GetWellNetwork to Amtelco’s On-Call Scheduling module, which keeps track of the nurses responsible for that patient’s room and messages the appropriate nurse with the result.
Early results showed a 48 percent average response rate from patients. “It is used in every inpatient area except for the critical care area,” Lorraine stated.
A time study revealed that checking on a patient takes a nurse 9 minutes. Susan Clark, RN Clinical Manager for the Float Pool at Valley Health said, “For a pain scale rating of 0 to 3, when the nurse doesn’t have to do anything since the patient’s pain is being controlled, it saved 69,066 minutes (1,151 hours) in a two-month period. For a pain scale rating from 4 to 10, where the nurse would have to do something, it saved 74,988 minutes (1,250 hours) within two months.”
Meeting Joint Commission Standards
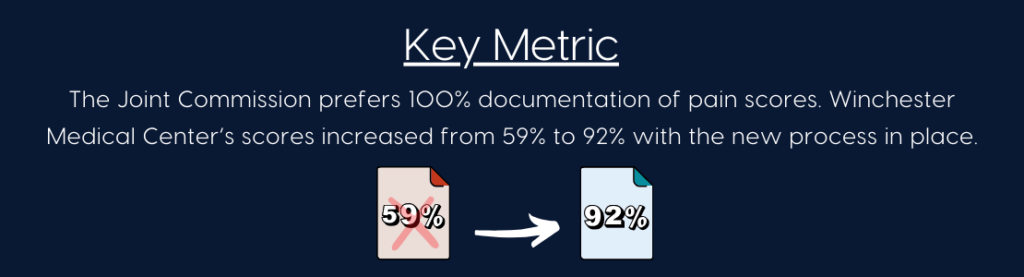
The Joint Commission staff was impressed with how the pain pathway was set up at Winchester Medical Center. The Joint Commission would like all healthcare facilities to have 100 percent documentation of pain scores. Winchester Medical Center’s scores were “originally around 59 percent and went up to 89 percent in documentation with the pain pathway. The scores have gone up to 92 percent with this system in place,” according to Lorraine.
“For a pain scale rating of 0 to 3, when the nurse doesn’t have to do anything since the patient’s pain is being controlled, [this integration] saved 1,151 hours in a two-month period. For a pain scale rating from 4 to 10, where the nurse would have to do something, it saved 1,250 hours within two months.”
Susan Clark, RN, Clinical Manager for the Float Pool at Valley Health
Winchester Medical Center quickly discovered what an effective process this was. When several departments didn’t copy the schedules for the nurses covering the patient rooms, the scores went down, giving them a way to prove that the pain pathway process was working.
Integration Benefits
Even though the process is automated, Winchester Medical Center still knows when something isn’t functioning exactly as they would expect. If a patient doesn’t respond to the GetWellNetwork pain level request, perhaps because their television is off, or the patient was asleep, the nurse receives a message that the patient did not respond so the nurse can check on that patient.
Although the nurses’ reactions to this new process were mixed, its benefits made it worthwhile. “Nurses don’t have to go to the patient’s room, get the medications, and then go back again. They are there only once, and that saves them a lot of steps,” said Lorraine.
Winchester Medical Center also uses the Amtelco notification system. “We are sending reminders out through Red Alert, reminding the nurses ‘to chart your medications,’” Lorraine said. Susan added, “That has brought up scores on some of the floors that are very busy and always turning over beds and patients.”